New Menopause Study Reveals Three Key Insights About Symptoms
Written by Dr. Brittany Barreto, Founder & CEO, FemHealth Insights
Menopause is a transformative journey that every female will experience at some point in their life. It is a natural biological process, yet it remains enigmatic, with symptoms and experiences varying widely among individuals. Phenology, a pioneering women's health brand from healthtech leader Hologram Sciences, has conducted an extensive survey of over 32,000 women to better understand their experience of menopause by stage. The results of this study provide invaluable insights into the complex transition of menopause, offering a deeper understanding of its stages and symptoms. In this article, we delve into three key findings that will revolutionize the way we perceive and address menopause.
Insight #1: There’s Nothing “Post” About Menopause
One common misconception about menopause is that once a woman reaches the postmenopausal stage, the most challenging symptoms are behind her. However, Phenology's research reveals that the reality is quite different. In fact, some symptoms are more pronounced during this phase of the transition.
Menopause is medically defined as the point in time 12 months after a woman's last period. This moment can happen at various ages, and being "postmenopausal" doesn't necessarily mean an end to troublesome symptoms. The Phenology study found that on average, women experience 9 different symptoms simultaneously throughout the peri and postmenopausal journey. But when you break down peri and postmenopause, women experience 7 and 11 symptoms, respectively. Again this shows that menopause is not just the experience of ending the menstrual cycle but symptoms persist and increase after menses end.
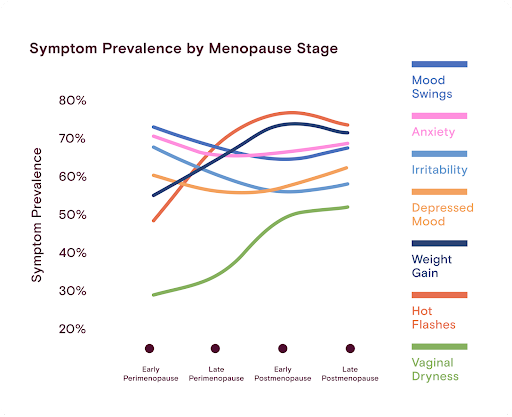
The data shows a strong correlation between age and physical and cognitive symptoms, with the highest occurrence of these symptoms in the late postmenopausal stage. For example, 77% of women in late postmenopause experience brain fog, compared to 70% in early perimenopause. Similarly, 73% of women in late postmenopause experience hot flashes, compared to only 39% in early perimenopause. The challenges are real and continue to affect women long after their last period. Sexual symptoms also peak in postmenopause, with 62% of women reporting low libido and 52% noting vaginal dryness, which can lead to painful intercourse.
The key takeaway from this insight is that postmenopause isn't the end of the road for managing menopausal symptoms. Women and their healthcare providers need to be aware of the persistent challenges faced during this phase and develop comprehensive strategies for managing them.
Insight #2: Perimenopause May Masquerade as Mental Health
The journey through menopause is a continuum, and it begins long before a woman's last period. Perimenopause, the stage preceding the official onset of menopause, is a phase marked by significant hormonal fluctuations. It's in this phase that women often experience emotional health symptoms that may be mistaken for mental health issues.
Phenology's study reveals that emotional health symptoms like mood changes, anxiety, and irritability are more prevalent in early perimenopause compared to the later stages of menopause. For example, 72% of women in early perimenopause reported mood swings.
Conversely, physical symptoms like hot flashes, night sweats, and sexual health problems become more pronounced in the postmenopausal stages. This finding challenges the prevailing narrative that menopause is primarily about hot flashes and night sweats.
These insights are consistent with the SWAN study, which found that women are more likely to experience major depression episodes during the menopausal transition. However, many women and their physicians in early perimenopause might not link their emotional symptoms to menopause, leading to under-recognition and under-treatment. Many women are referred to psychologists when they in fact need menopause treatment.
Furthermore, a lack of comprehensive menopause education among healthcare providers, as shown by the fact that only 31% of OB-Gyns undergo formal menopause curricula, exacerbates this issue. It's vital for both women and their healthcare providers to recognize the unique challenges of perimenopause and respond accordingly and stop outsourcing menopause to therapists as solely a mental health issue versus a symptom triggered by hormonal fluctuations.
Insight #3: No Two Menopause Journeys Are the Same
Perhaps the most striking revelation from Phenology's research is that no two menopause journeys are alike. Women experience the transition through menopause with widely varying symptoms and timelines. This also means there cannot be one solution for all of menopause.
First, women are entering menopause at different ages, with some starting their transition at 50 while others are post-menopausal by that point.
Age ranges for each stage of menopause, showing the 5th through 95th percentile overall, with emphasis on the 25th-75th percentiles.
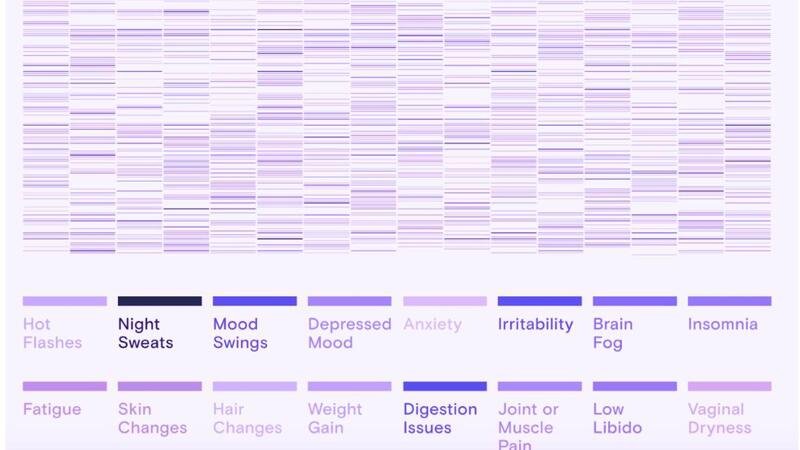
The study showed over 15,000 unique symptom combinations reported among the 32,000 women surveyed. This makes it clear that there is no consistent symptom pattern during menopause; each woman has her own symptom “signature.”
A random sample of 200 women in the study illustrates the variation of menopause symptom signatures.
Given the high degree of individual variability, innovation must take an individualized approach to support women and women must be their own advocates when identifying solutions for their specific symptoms. Moreover, it's disheartening to learn that 50% of women are not treating their menopausal symptoms when accessible solutions exist. This may be a result of not knowing what they are experiencing is menopause, a lack of access to solutions, or a resistance to acknowledge their condition due to stigma.
Of those who do seek treatment, most are adopting a holistic approach, combining multiple strategies for relief. These strategies include nutritional changes, non-hormonal supplements, exercise, and alternative therapies such as massage and acupuncture. The diversity of approaches underscores the importance of personalized care during the menopausal transition.
For example, Phenology provides 1:1 coaching from a menopause-trained registered dietician who can help each woman adopt simple lifestyle strategies to address her particular symptoms such as cutting out caffeine and red wine to reduce hot flashes. Individual attention and support for habit changes are key to helping women reduce symptoms.
Conclusion
Phenology's comprehensive study provides crucial insights into the complexities of menopause. Women should be aware that the challenges of menopause persist well into the postmenopausal stage, emotional health symptoms during perimenopause are common, and every woman's menopause journey is unique.
With a personalized, holistic approach to treatment, women can navigate this transformative life stage with greater ease and enhanced quality of life. Additionally, healthcare providers should strive to better understand the nuances of menopause and provide tailored support and guidance. By embracing these key findings, we can revolutionize our approach to women's health during the menopausal transition, ensuring that no woman is left to navigate this journey alone.
About the Author:
Dr. Brittany Barreto, Ph.D., is Founder and Chief Innovation Officer at FemHealth Insights. Every day, Brittany dedicates her work to advancing women’s health innovation by equipping key stakeholders with data-driven insights and strategic advice on the FemHealth market. She is also host of the FemTech Focus Podcast - the number 1 femtech podcast globally.